South Africa’s HIV epidemic is maturing, with more older people living longer on antiretroviral therapy. However, young people are still at risk. According to the HSRC’s sixth HIV household survey, a summary report of which was released in November, less than half of young people with multiple sexual partners are using condoms while they are least likely to be virally suppressed. Findings such as these have public health implications and emphasise the continued relevance of this flagship HSRC survey series, which is celebrating more than 20 years of tracking HIV in South Africa. By Antoinette Oosthuizen

Photo: HSRC
South Africa’s population of older people living with HIV has increased, probably because antiretroviral therapy (ART) is allowing people to live longer and healthier lives with HIV. Their changing healthcare needs will require an integrated treatment approach, which also considers age-related non-communicable diseases and mental health. At the same time, prevention programmes will need to be stepped up among young people, since many are still not using condoms despite this having been the focus of many HIV awareness programmes for over two decades.
This was revealed by experts at the recent launch of summary findings from the HSRC’s Sixth South African National HIV Prevalence, Incidence, and Behaviour (SABSSM VI) survey.
An ageing population with HIV
SABSSM VI found the percentage of all people living with HIV (PLHIV) in South Africa to have decreased from 14% in 2017 to 12.7% in 2022.
“Several factors contribute to HIV prevalence,” said Professor Khangelani Zuma, divisional executive of the Public Health, Societies, and Belonging division of the HSRC and overall principal investigator of SABSSM. “These include fewer people getting infected with HIV, more children born HIV negative, less AIDS-related mortality, and people ageing and dying from natural causes. The increase in the population (birth of HIV-negative babies) would also increase the denominator of HIV-negative people in the country.”
The researchers also noted a shift in HIV prevalence peaks between 2017 and 2022, indicating an ageing epidemic, as more people on ART survive into old age.
Among men, in 2017 the peak prevalence was 26.7% in those aged 35–39 years (Figure 1), while in 2022 the peak was 27.1% – but among those aged 45–49 years. The drop in prevalence in the younger male age groups may indicate that new infections (incidence) have decreased. Incidence data is still being processed and will be released in the final SABSSM VI report early in 2024.
Figure 1. Overall HIV prevalence among men in South Africa, 2017 vs 2022
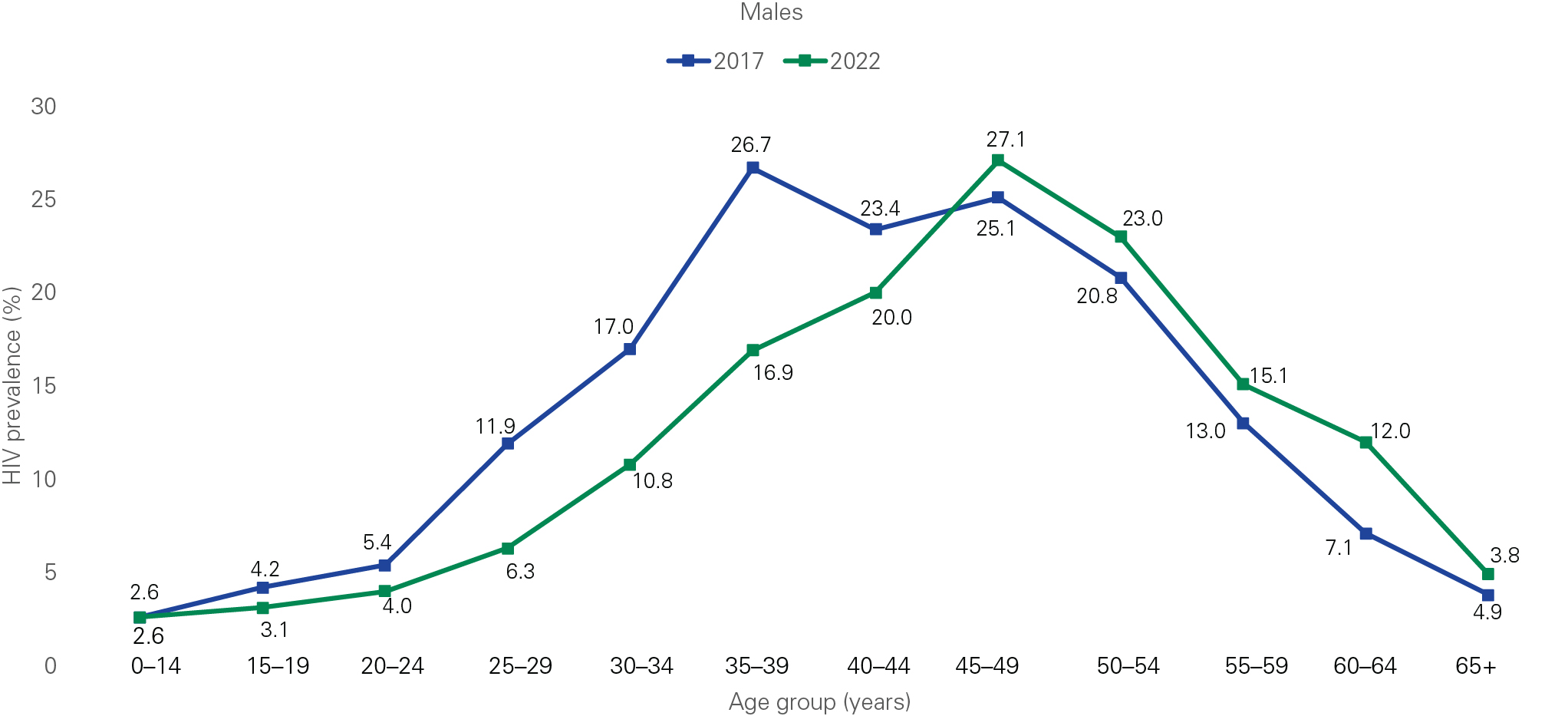
Source: SABSSM VI
At the launch, Dr Eva Kiwango, UNAIDS Country Director, said the shift in age distribution means programmes will need to consider the changing care needs of PLHIV. Many of those in the older age groups live with other chronic conditions and the shift has implications for integrating HIV and other health services, such as those for non-communicable diseases and mental health.
Zackie Achmat, co-founder of the Treatment Action Campaign (TAC) 25 years ago and known worldwide for his HIV and AIDS activism, also highlighted the plight of elderly PLHIV in a recent interview with the HSRC.
“We [need to] understand what is happening to people like me who are in our 60s and going into our 70s … because the people on treatment are those who are born with HIV, right through to those of us who’ve had HIV [for decades].
“We need studies of comorbidities and the impact on geriatric AIDS, the psychological and mental health needs of PLHIV, because there’s still a certain stigma around it … you feel lonely and the fact that you have to take pills every day … [the] sense that you never leave HIV, [like] you leave the flu or COVID-19.”
Achmat believes that messages should focus on drug adherence and HIV prevention, but also emphasise the positive. “We need messages from older people who say, ‘I’m healthy but now these are my problems. But I couldn’t have looked after my grandchildren if I didn’t stick to my medication.’”
Women still bear the brunt
Among adults aged 15+ years, HIV prevalence was nearly twice as high among women (20.3%) compared to men (11.5%). By race, HIV prevalence was highest among black people (19.8%), followed by coloured (5.1%), white (1.3%), and Indian/Asian (1.2%) people.
Among women, HIV prevalence was highest in the age range 35–39 years at 34.2%, whereas among men it was highest in those aged 45–49 years at 27.1% (Figure 2). Pronounced differences in HIV prevalence by sex were seen among younger populations, with it being approximately twice as high in young women aged 15–19 years (5.7% vs 3.1%) and 20–24 years (8% vs 4%), and three times higher in women aged 25–29 years (19.5% vs 6.3%) compared to in men.
“It is shocking that in 2022, with all that we know, we have age groups of women where the prevalence is three times higher than in men,” said Dr Thembisile Xulu, CEO of the South African National AIDS Council, at the launch of the summary report.
Zuma says the vulnerability of women has been a persistent challenge over many years and partly relates to young women having sexual relations with older men.
Figure 2. HIV prevalence by sex and age in South Africa, 2022
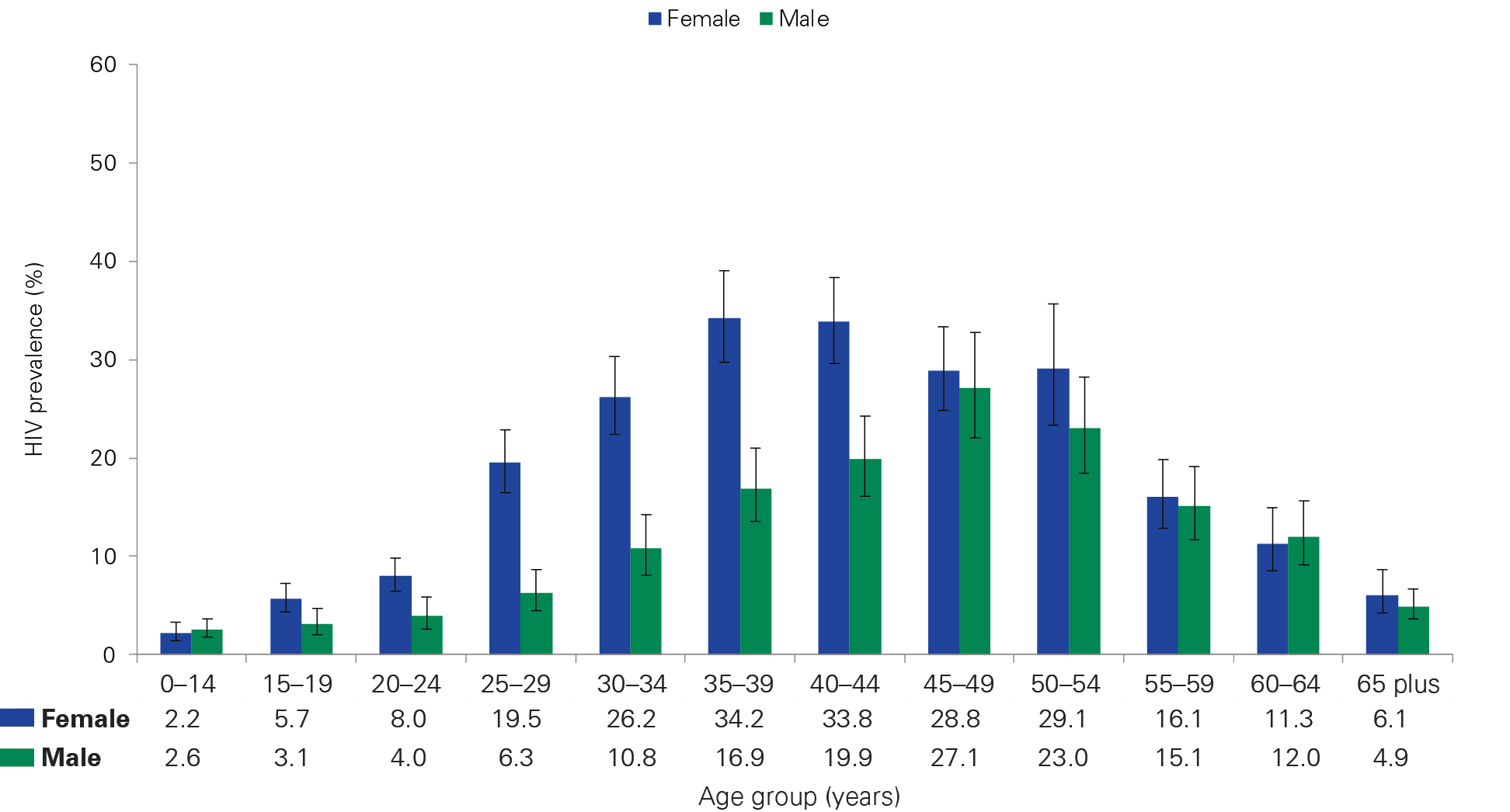
Source: SABSSM VI
Viral load suppression
ART reduces the amount of HIV in the body (viral load) in those who test positive for HIV. Having less than 1 000 copies of HIV/ml blood means viral load suppression (VLS) has been achieved, and the person’s chance of getting ill or transmitting HIV is reduced.
SABSSM VI showed that VLS among adults aged 15+ living with HIV had increased from 62.2% in 2017 to 81.2% in 2022 (Table 1).
It was the highest in females (91.4%) aged 55–64 years, followed by males aged 65 years and older (86.9%). VLS was lower among younger adults, being lowest among women aged 15–24 years (68.2%) and men aged 25–34 years (66.3%).
Table 1. Viral load suppression among people living with HIV by age and sex in South Africa, 2017 and 2022
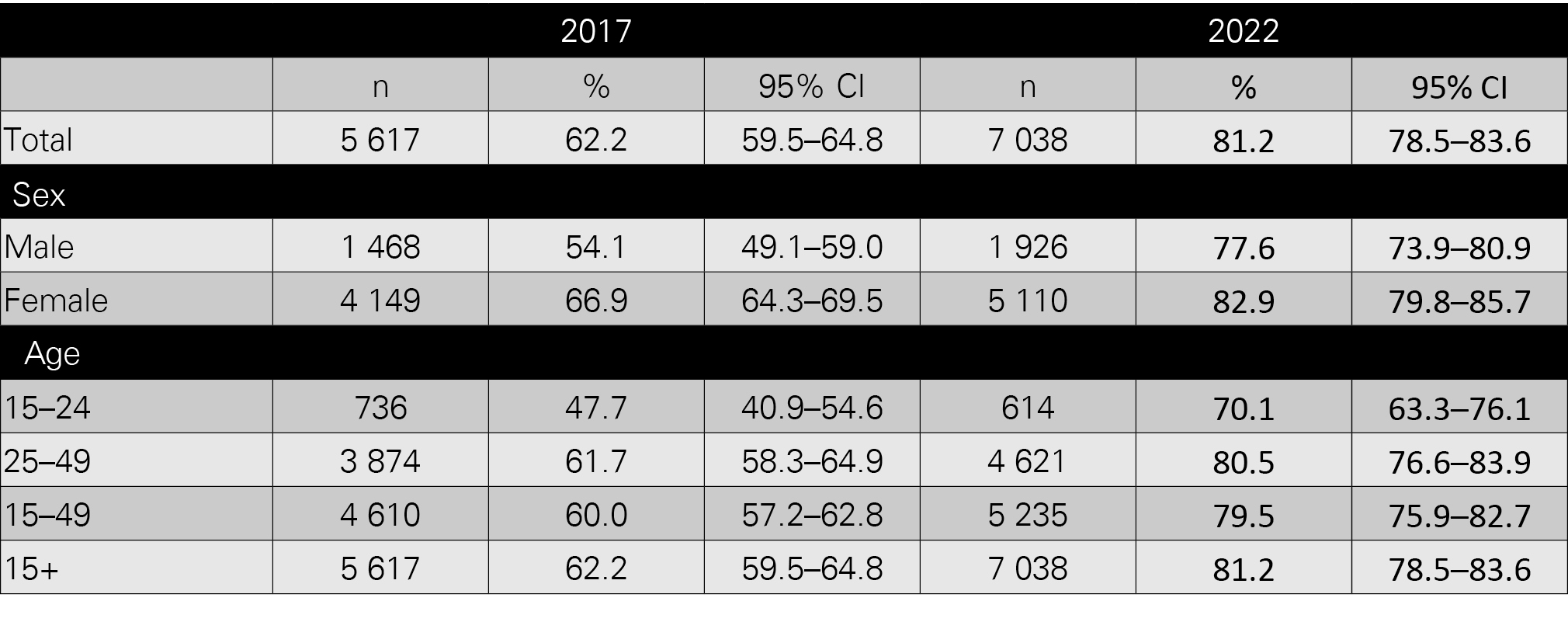
Source: SABSSM VI
Condom use
SABSSM VI also asked participants who had more than one partner in the previous year about condom use the last time they had sex. Among those aged 15–24 years, 50.6% of men and 43.5% of women said they had used condoms. Among older adults aged 50 years and older, self-reported condom use was 27.9% among men and 29.0% among women (Figure 3).
Figure 3. Condom use during most recent sexual encounter for people with multiple sexual partners in South Africa (2022)
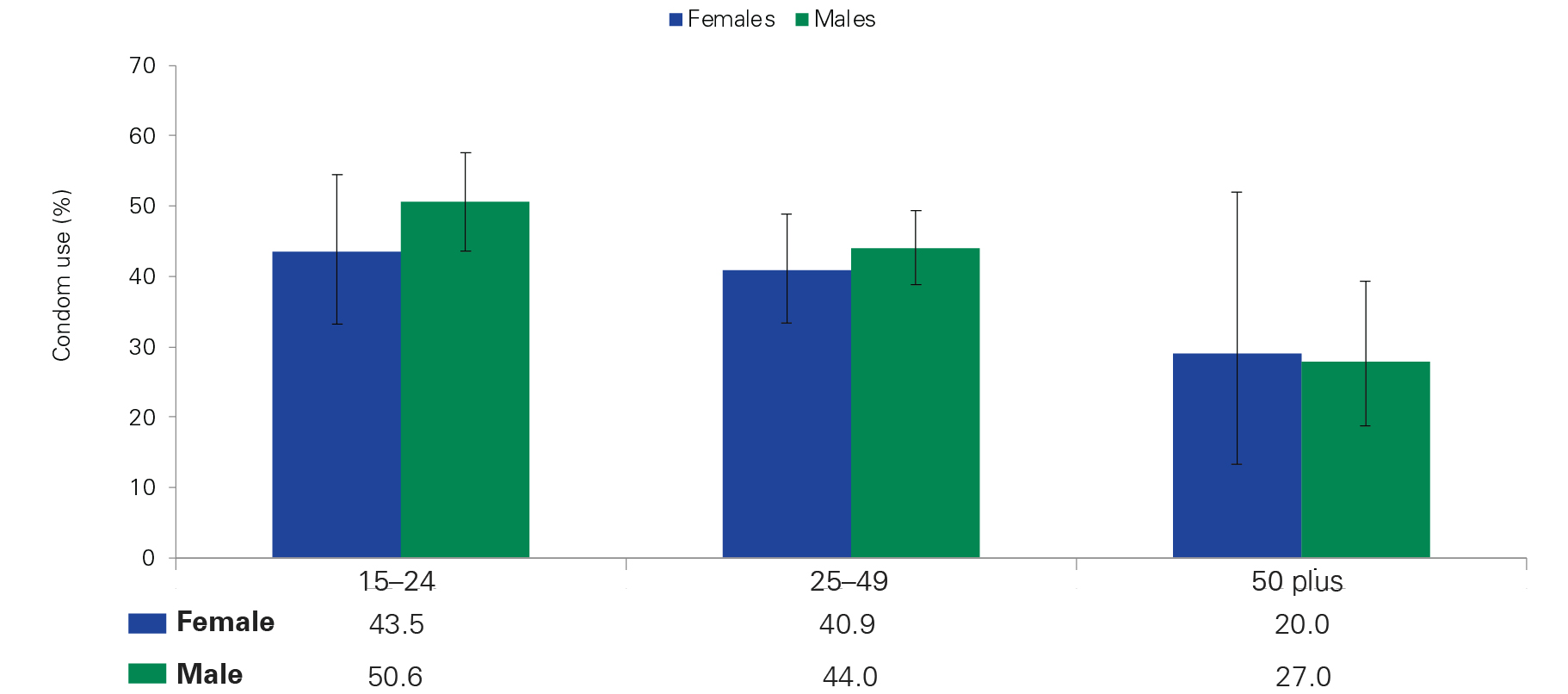
Source: SABSSM VI
Youth at risk
Zuma warned that while HIV prevalence decreased to 390 000 of those aged 0–14 years and 533 000 of those aged 15–24 years, the numbers are still concerning, as many young people may not know their HIV status. Their lower VLS means they can spread HIV more easily, and half of young people with multiple partners don’t use condoms.
Achmat believes new messages need to target the youth.
“[We have] young people living with HIV and taking medicines. … We may not find many who are willing to be open, but the ones that can, should be able to speak of their struggle. Most importantly, they should be able to speak about how they’re healthy and can’t transmit HIV [due to VLS].”
Reaching 95–95–95
South Africa has made progress on its 95–95–95targets – that by 2025, at least 95% of all PLHIV will know their HIV-positive status; 95% of those diagnosed HIV positive will be on ART, and 95% of all those on ART will have achieved VLS.
SABSSM VI shows that in 2022, 90% of PLHIV aged 15 years and older knew about their HIV-positive status (92% of women and 85% of men). Of those who knew their HIV status, 91% were on ART (91% of women and 90% of men). Overall, 94% of those on ART were virally suppressed (Figure 4).
This is an improvement compared to 2017, when the UNAIDS target was 90–90–90 but South Africa achieved 85%–71%–87%. The great uptake of treatment can be attributed to the changes in treatment guidelines in 2016, explained Zuma. The new guidelines made provision for everyone requiring HIV treatment to be given it immediately, regardless of their clinical status, which previously needed to include a CD4 count below 500 cells/mm3.
Figure 4. 95–95–95 indicators for people aged 15 years and older living with HIV in South Africa, 2017 and 2022
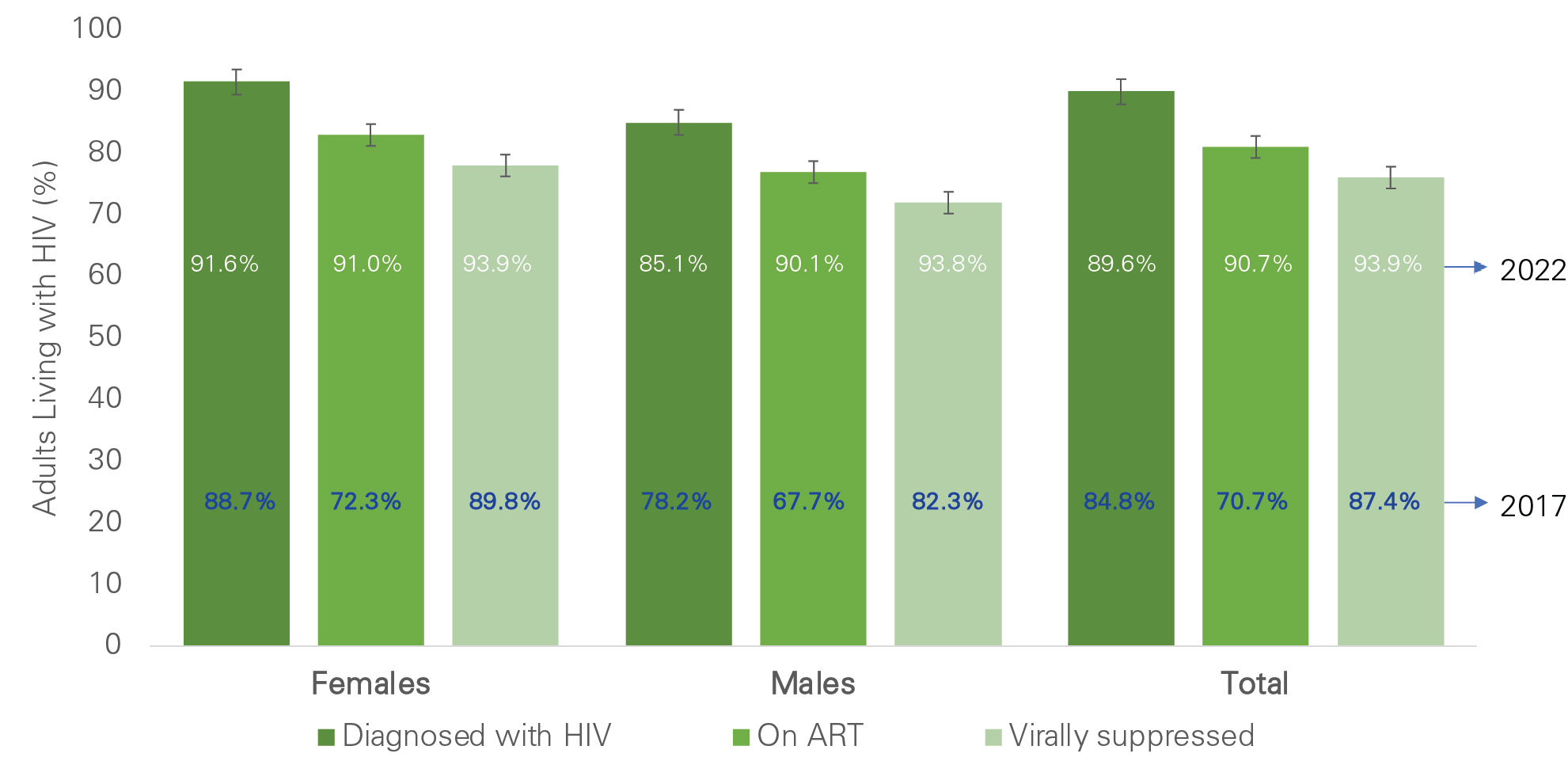
Source: SABSSM VI
History: SABSSM changes over the years
The HSRC, in collaboration with a consortium of partners, has been implementing SABSSM surveys for the past 20 years, starting with the 2002 Nelson Mandela/HSRC-funded survey on HIV and AIDS, followed by the 2005, 2008, 2012, and 2017 surveys. The 2022 survey was the sixth in the series.
The SABSSM surveys have become a major source of information for measuring progress in the implementation of South Africa’s national strategic plan to curb HIV, sexually transmitted infections, and tuberculosis.
Over the years, the researchers have increased the number of biomarkers measured, expanded participation to entire households, and introduced electronic data collection systems, which allow them to access data immediately. The first survey included 9 963 participants and focused on estimating HIV infection, prevalence (cumulative HIV infection cases), incidence (new HIV cases), and knowledge, attitudes and perceptions about HIV and AIDS and sexual behaviour.
The sixthsurvey is the largest to date and was expanded to collect data on SARS-CoV-2, the virus that causes COVID-19. Researchers approached 76 134 people in all 9 provinces and 62.7% agreed to provide blood specimens. It is hoped that once available, the new data on COVID-19 will also help to inform South Africa’s future pandemic response policies and interventions. The HSRC is finalising the main SABSSM VI report, which is expected to be released in April 2024. It will also include an analysis of new HIV infections (incidence) as well as summary sheets with data for provinces and selected districts.
Impact: The importance of good data
“This survey began to make HIV real,” said Professor Salim Abdool Karim, associate scientific director of the Centre for the AIDS Programme of Research in South Africa (CAPRISA), when recently interviewed by the HSRC.
“I have always felt that the first survey was a turning point in the way in which the public understood this pandemic and the way in which they grappled with the evidence.”
Achmat also believes that good data has been crucial in the decades-long struggle against HIV and AIDS in South Africa.
“In the TAC, we always said the first place to start is the fundamental rights of everyone to life, healthcare, dignity, and equality. Once you’ve set your principles, the second place you go is to evidence – research and data – to see what needs to be done, and what should not be done. That’s what science is. From there, you educate yourself, the activists, and the public. Research work – the work of gaining knowledge – is essential for justice. You cannot have justice without knowledge.”
Achmat praised the numerous scientists and health workers who spoke truth to power at great personal risk during the difficult years of HIV denialism in South Africa: “They not only used their science and knowledge to improve lives but were morally invested in what they’re doing.”
The way forward
In a recent interview with the HSRC Dr Olive Shisana, special adviser to President Cyril Ramaphosa and former HSRC CEO, warned that continued funding of SABSSM is more critical than ever.
“We continue to have the largest number of people with HIV in the world … failing to provide funds to prevent HIV does not mean that the problem is going to remain in Africa. People’s bodies are biological hazards. They travel from one place to the other … it is very important that [we have] resources to make sure that we do not have the epidemic continuing to become a pandemic … so that we end AIDS itself [and] so that no one should ever have to die of AIDS.”
SABSSM contact: SABSSMVI@hsrc.ac.za
SABSSM VI was led by the HSRC in collaboration with partners and was conducted with funding from the US President’s Emergency Plan for AIDS Relief (PEPFAR) with technical collaboration with the Centers for Disease Control and Prevention, South African Medical Research Council, NICD, University of Cape Town, South African National Aids Council, and UNAIDS.


