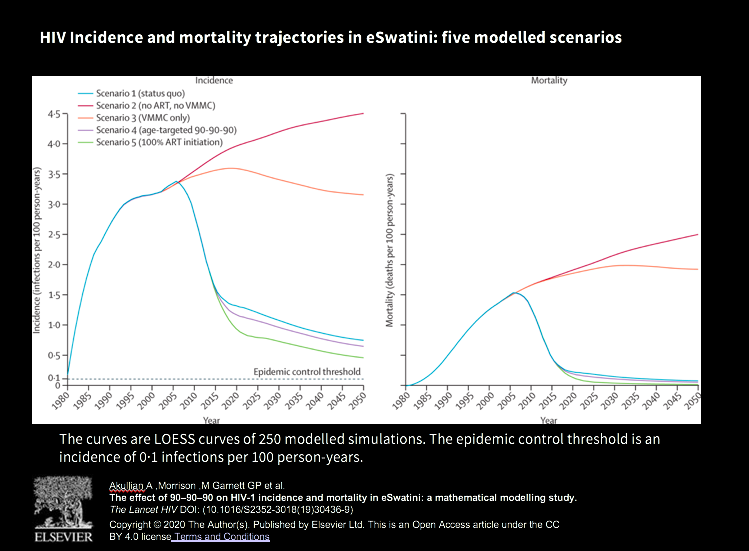
Although the contribution of each component of the HIV response is not known, one mathematical model published in February 2020 in the Lancet found that the intervention contributed modestly to short term reductions in new infections, with the effect expected to increase over time, assuming 2016 rates of coverage (see the figure above). As expected, the overall impact on HIV incidence reductions was bigger for men than for women. The study notes that if greater coverage is achieved, these projections will underestimate the impact on new infections.
With 90% of adults aware of their status in 2017, South Africa has also made progress towards its 90-90-90 goals. However, it has also missed its circumcision targets, with 32% (compared to an intended 80%) of men circumcised in 2017. Rates are highest among young men (ages 15-24) among whom almost half (43%) have undergone VMMC.
At the book launch, Nqeketo emphasised the importance of clear and culturally sensitive communication and argued the need for reflection. “I’m calling on my former colleagues in eSwatini to say, let’s reflect together. I’m calling on my former colleagues in South Africa and any other country in Southern Africa… let’s see how we can improve.”
With a 60% lower risk of female-male HIV transmission, the cost-effective intervention has been recommended by the WHO and public health experts, as particularly suited to regions, like South Africa and neighbouring eSwatini, with high HIV prevalence. However, medical male circumcision remains controversial, and realising these HIV transmission reduction benefits requires overcoming cultural, behavioural and political challenges.
In eSwatini, more than 1 in 4 adults are living with HIV. While prevalence has now stabilised (and in fact has decreased slightly), the turnaround has only come in the past decade, with the rapid scale-up of antiretroviral treatment (ART). In 2011, incidence was estimated at 25 new infections for every 1000 people – translating into 12 000 new infections per year.
Neighbouring South Africa was similarly struggling under the weight of the epidemic: with a much bigger population, its 16.6% prevalence (for 2011) translated into 5.4 million people living with HIV AIDS. (Today, prevalence sits at an estimated 20%, or 7.7 million people.) However, when it came to rolling out circumcision, South Africa arguably had an advantage.
Circumcision was already an accepted and widespread cultural initiation practice: voluntary medical circumcision could piggyback on tradition. (Of course, there were and are challenges: for example, some isiXhosa men believe that circumcisions conducted in a clinic do not confer the status of manhood.)
In eSwatini, however, circumcision not a cultural practice. In fact, Nqeketo said, speaking at the HSRC-hosted launch of his book, The Controversial Cut | rolling out mass male circumcision in Eswatini, it was an identifying feature that actively set Swazi men apart from their South Africans neighbours.
An anthropologist with experience in scaling up circumcision in South Africa, Nqeketo was charged with heading up the effort to increase uptake of the intervention. An isiXhosa man, raised in a village in the Eastern Cape, South Africa, Nqeketo was acutely aware of the importance of understanding the local context and working with traditional leaders to deliver a culturally sensitive intervention. A successful scale-up, he realised, would require bringing together very different stakeholders – public health experts, traditional leaders religious leaders, boys – towards a common goal.
As the reported failure of the first campaign showed, this was challenging. Myths and misinformation were rife: for example, one rumour maintained that discarded foreskins had been found in stock cubes. To dispel misinformation, Nqeketo and his colleagues visited schools and villages and authored explainer articles in local eSwatini newspapers.
Meanwhile, public health professionals faced the challenge of ensuring that men volunteering for the circumcision understood the benefits and the limitations. One public health concern regarding voluntary circumcision is risk compensation, where behaviour change offsets the expected benefits: in this instance, the possibility that circumcised men – knowing that they are partially protected from acquiring the virus – respond by engaging in more risky sexual behaviour, putting their partners at higher risk.
A related poorly understood element of circumcision is that circumcision reduces female to male transmission but is not protective for women — if a circumcised man acquires HIV, the fact that he is circumcised will not reduce his partner’s risk for infection. This is particularly pertinent in eSwatini, where women are at much greater risk for infection: 35.1% of women and 19.3% of men are living with HIV.
So is the worry that circumcised men engage in riskier behaviour founded? A 2012 South African Medical Journal editorial argues that this risk has been overstated: while one study in South Africa found that men in the intervention group engaged in slightly riskier behaviour, others, for example in Uganda, found no evidence for this effect, possibly due to extensive counselling and educational components. Public health experts have stressed the importance of ensuring that men do not receive a distorted message that circumcision confers 100% protection.
According to Nqeketo, the limitations and benefits of circumcision in relation to risk for HIV/AIDS and other STIs are clearly communicated to men in comprehensive counselling sessions when they undergo circumcision.
Today, eSwatini has achieved significant circumcision roll-out, although coverage – at an estimated 35% — remains lower than current targets. With 86% of all people living with HIV on treatment (and, of those on treatment, 94% of those virally supressed), the country has made impressive strides towards containing the epidemic. Between 2011 and 2016, incidence almost halved, from 2.5% to 1.7%.
In the wake of the disappointing news of the ineffectual new HIV vaccine, medical male circumcision remains the only once-off intervention that reduces the risk of acquiring HIV. Yet in both Swaziland and South Africa, in the absence of clear communication and the support of opinion leaders, much of this benefit may be lost. At a recent HSRC book launch, Ayanda Nqeketo, founder of the Ikamva Lesizwe Institute, spoke about the challenges in rolling out MMC in Eswatini – and how some of these lessons might be applied to South Africa.


